This is a self-indulgently long story. The gist of it is that my wife, Rachel, was unexpectedly induced due to gestational hypertension at 37 weeks, right before we were supposed to head to Pennsylvania for her sister’s wedding.
After a lengthy induction and labor, our beautiful daughter, Eva Joy Steele, was born at 5:46am on Friday, July 20, 2018.
If that’s all you’d like to know, great! If you’d like to know more about what went down, keep reading.
Here’s a cute picture/tweet for your troubles.
(NOTE: The Twitter embeds/links below no longer work. Apologies! But I’m keeping them in for posterity.)
It all started on Tuesday, July 17, 2018.
The main thing I had scheduled that day was a get-together with my doctoral supervisor and his other students to discuss part two of our reading of Friedrich Schleiermacher’s Christian Faith.
As per usual, before diving into our book discussion, we went around the table and gave life updates. The gist of mine was:
Well, we had a bit of a “scare” last week, because Rachel’s blood pressure was slightly elevated at her midwife appointment. So, they sent us over to get an NST (fetal non-stress test), more blood pressure measurements, and an ultrasound to measure the baby.
Thankfully, everything looked fine. We’re pretty sure her high blood pressure is due to “white coat hypertension,” because her BP always looks fine at home and at work.
So, we’ve got another midwife appointment this afternoon, but we should be all set to drive out to Pennsylvania tomorrow for the wedding this weekend.
~Me.
You see, on Saturday, July 21, Rachel’s sister, Hannah, was getting married. Rachel was the Matron of Honor, and I was the officiant for the wedding.
Or at least, that’s what we were planning on.
The Midwife Appointment (4:00 pm, Tuesday)
I met Rachel at Elmhurst Hospital for our midwife appointment on Tuesday afternoon.
Just like the previous week, her initial blood pressure was high. So, they sent us over to triage on the Labor and Delivery unit for another NST.
“No big deal,” we thought. “Things will come back normal again, and we’ll be on our way to Pennsylvania tomorrow.”
In fact, while Rachel headed over to triage, I went out to pick us up some food for dinner.
Triage, Elmhurst Hospital, Labor and Delivery Unit (˜5:00pm, Tuesday)
When I got over to the triage room, Mediterranean pita wraps in tow, Rachel was already hooked up to the monitors.
Unfortunately, more than two of her BPs were higher than 140/90. To us, this didn’t seem like that big of a deal. Surely it was just a combination of nerves and stress!
However, Rachel met the diagnostic criteria for gestational hypertension. And, as a midwife explained to us in the triage room, the treatment for gestational hypertension these days is to induce labor starting at 37 weeks gestation.
Which, for us, meant getting induced in about 7 hours, shortly after midnight. The only other alternative was to leave AMA: “Against Medical Advice.”
To put it lightly, this was difficult news to receive. We went from thinking that we were going to be on our way the next day to Pennsylvania for the wedding to realizing that we were going to be in the hospital until we came home with a baby!
So, first, there was the disappointment/stress of missing the wedding. Then, there were the other questions: Were we ready for the baby to arrive? (The nursery wasn’t due to be finished until around August 8, the due date.) Was Rachel’s body ready to deliver at 37 weeks? Was this labor and delivery more likely to end in a C-section? Would the baby be OK, or would she face health complications from being born too early?
The midwife reassured us that the baby was not going to be significantly more likely to have health complications from being delivered at 37 weeks vs. waiting to 38 or 39 weeks to induce labor.
On my end, it was helpful to hear that the reason gestational hypertension is a concern, even though it’s not as serious as pre-eclampsia, is that the mother’s blood pressure can very quickly and unexpectedly get out of control late in the pregnancy. There’s no way of telling on the front end, however, which mothers/babies will be fine all the way through and which will die unexpectedly. So, inducing labor at 37 weeks across the board for gestational hypertension has been determined to be the safest course of action.
So, while it was going to be a bummer to miss the wedding, I reassured myself/Rachel that, at least, we would get to meet our baby girl soon! Plus, even if we had been able to sweet-talk our way into a deal where they let us go home and come back for blood pressure checks each day, I wasn’t sure that “freedom” would be worth the extra stress.
Admitted to Elmhurst Hospital, Labor and Delivery Unit (˜7:00pm, Tuesday)
So, we literally walked right across the hallway from triage to our pre-partum hospital room on the Labor and Delivery unit.
After getting settled, we began the process of letting friends and family know what was happening.
I let my doctoral supervisor and fellow students know that I had spoken too soon that afternoon, and that we wouldn’t be making the trip out to Pennsylvania.
I also let our landlord know that we would be needing that baby room finished sooner than initially expected!
And, as I headed back home to grab supplies for our stay at the hospital, I called my parents to let them know that their granddaughter would be arriving sooner than expected.
Back at the apartment by myself, calling Rachel to double-check what she needed in her “go-bag,” it was a bit surreal to realize that, most likely, the next time I would come home we would have our daughter with us!
I somewhat frantically tidied-up the apartment (“I don’t want our baby to come home to a messy house!”) and packed our bags before heading back to the hospital.
INDUCTION STARTS: Cervidil (˜12:30 am – 12:30 pm, Wednesday)
The induction process started around 12:30 am with the insertion of a medicine called Cervidil to soften the cervix.
Despite our hopes that things would start to progress rather quickly, Wednesday was a looooooong day. Looking back, I can tell that this was the case because I had time to tweet.
Also, I figured that now was as good a time as any to ask for some last-minute parenting advice.
By the way, my friend Ryan Clevenger wins the award for best dad advice given in response to my tweet.
Anyways, the first round of Cervidil lasted 12 hours. After they took the Cervidil out, they checked and Rachel was barely dilated.
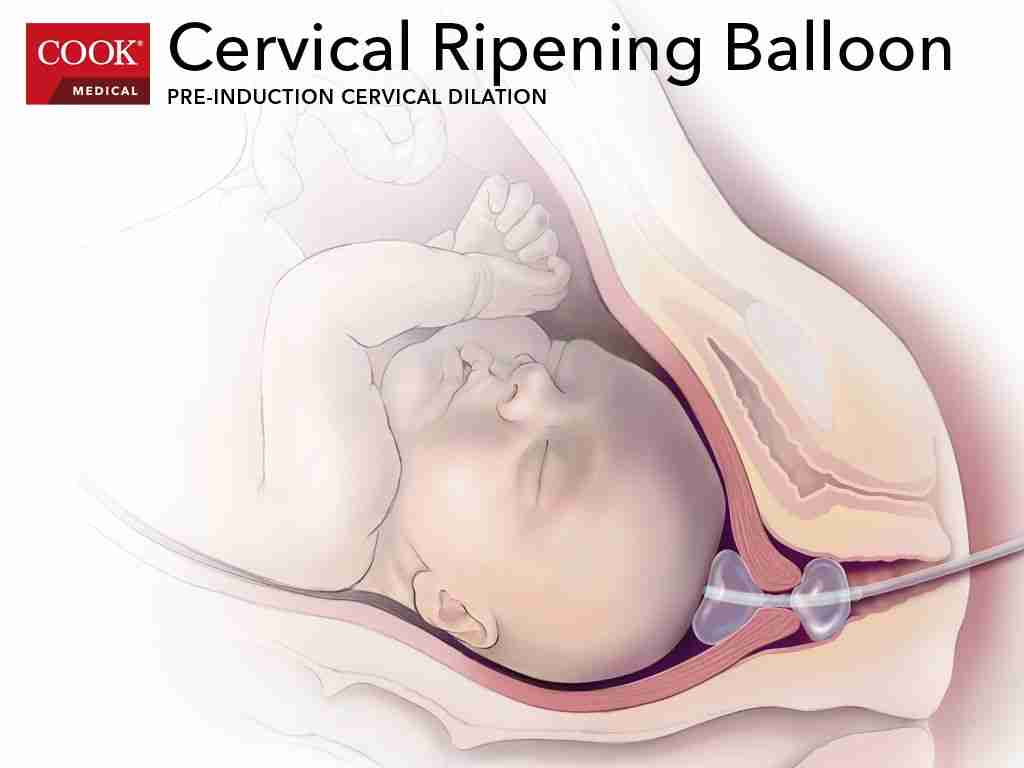
Nevertheless, they decided to try to insert what is called the Cook Cervical Ripening Balloon, AKA the Cook catheter.
Cook Cervical Ripening Balloon, Unsuccessful Attempt #1 (1:30 pm, Wednesday)
Here’s a picture of what we’re talking about.

They insert that thing through the cervix, before inflating those balloons on both sides of the cervix.
Or, at least, that’s how it’s supposed to go.
Unfortunately, they weren’t able to get this thing in on Wednesday afternoon. According to Rachel, it was extremely painful. It was difficult to watch her go through it.
So, after giving her a bit of break, the midwife recommended starting Pitocin.
Started Pitocin (4:00pm, Wednesday)
After the unsuccessful insertion of the Cook catheter, they decided to monitor Rachel to see if any regular contractions started. No dice.
After talking with our doula, Teri, on the phone, we decided to start Pitocin on Wednesday afternoon. If you’re curious, here’s some more information about Pitocin and what it does.
So, they started Pitocin at around 4:00pm on Wednesday. Just like Cervidil, the first round lasted approximately 12 hours.
To Eat, or Not to Eat
Apparently, normal hospital protocol is that you’re only allowed to consume clear liquids while on Pitocin. We’d heard from various people that this was a load of crap. However, the midwife who was there when we started Pitocin still said “clear liquids only.”
Nevertheless, we still snuck Rachel snacks when nurses weren’t in the room!
On Wednesday evening, we met with a different midwife to discuss how things were progressing. She said “You’re eating, right?,” and then we told her about our clear liquid instructions.
“No no no, you (looks at me) go get her some dinner, OK?”
Best. midwife. ever. I went and got Rachel some Pad Thai.
We also discussed with the midwife what would happen if things didn’t progress at all over night. She said that, if NOTHING had changed in the morning, that they would consider another consult with maternal and fetal medicine doctors to see if we could be sent home for 24 hours before returning to re-start the induction process.
However, she said, if things had moved along enough to allow for the insertion of the Cook catheter, then we would proceed until the baby arrived.
Off Pitocin (5:30 am, Thursday)
At around 5:30 am, Rachel came off her first round of Pitocin. They checked, and she was only dilated to 1cm. This was kind of a bummer. 29 hours after induction began, with only a measly centimeter to show for it!
Nevertheless, this was still progress. So, the next thing we decided to try was the insertion of the Cook catheter again.
Before doing so, Rachel got another break, during which she drank some coffee, ate breakfast, took a shower, etc. Honestly, she seemed pretty chipper at this point. Which was good, because things were about to get going!
LABOR STARTS: Cook Catheter, Successful Attempt #2 (8:30 am, Thursday)
Thankfully, the second time was a charm. They were able to successfully insert the Cook catheter on Thursday morning at 8:30. (Although, it took another three tries. According to Rachel, the first two were quite painful but the third, when it was successfully in place, didn’t feel that bad.)
After this, however, Rachel started feeling worse/bad and contractions started to pick up. From my perspective, the difference between Rachel at 8:00am and Rachel at 10:00am was enormous.
Looking back, we’d say that labor started around this time.
Unfortunately, what also started around this time was vomiting (Rachel, not me). I wrote down the first times: 0912, 0945, 1050, 1121, 1215, 1430, 1605… Then, in my notebook, I just have “… (more times).” It was rough.
Back on Pitocin (10:30 am, Thursday)
Things were progressing, but they didn’t exactly take off after the Cook catheter was in. So, it was back on Pitocin.
Rachel’s contractions were getting more and more painful. Specifically, she was complaining about pain/tension in her lower back.
What’s more, she was getting to the point where she had to stop talking during contractions. This despite her insistence that, while she could talk through the contractions if she really wanted to, it was easier not to talk…
Between that and the vomiting, I suggested that we give our doula a call and ask her to come in.
Doula Teri Arrives (1:00 pm, Thursday)
Teri, our doula, arrived at about 1:00 pm on Thursday. Rachel wasn’t doing so hot by then, and I was very glad to have someone else there for more support.
The way things were going, with the back pain and the vomiting, I wasn’t sure how much longer we’d be able to handle things on our own without someone a bit more knowledgeable there to support us.
Turning Babies, Stressful Nurses (Thursday Afternoon)
Thanks be to God that Teri came when she did!
With some coordinated hip movements, she was able to turn the baby around and relieve Rachel’s back pain! Rachel said that it was the weirdest thing ever feeling the baby turn around, and it brought pretty much instant relief.
So, even though her contractions kept getting more intense, they were easier to bear without the pain being concentrated in her lower back.
Nevertheless, Thursday afternoon wasn’t all rainbows and butterflies.
For one thing, despite the relief in back pain, contractions were still picking up. At one point, they were about 2.5 minutes apart and pretty intense.
However, we got a new nurse at this point, and she really just stressed us out. She meant well, to be sure, but her ways of handling things were quite different than any of the other nurses we had throughout the process.
Whenever she would come into the room, which she did rather frequently, Rachel’s contractions would slow down or get erratic. This made the nurse (and the midwife) want to crank up the Pitocin. It wasn’t the greatest afternoon.
However, that nurse eventually left. Also, Rachel was able to get a decent nap in… THROUGH some pretty intense contractions! (Teri and I were pretty surprised, looking at the monitor, watching the contractions come, without a peep or change in facial expression from Rachel as she slept.)
Removed Cook Catheter (8:00pm, Thursday)
There’s something about 12 hour rounds of things during induction/labor. So, at 8:00pm or so, they took out the Cook catheter.
After a pretty intense afternoon, Rachel was dilated to (*drumroll*) … 3cm!
43.5 hours for 3 centimeters. Sure, progress. But SLOW!
The midwife recommended breaking the bag of waters to move things along. After being reassured that this wouldn’t put us “on a clock” before they would intervene with a C-section, we decided to go ahead with that plan.
Broke Bag of Waters, Transferred to Labor and Delivery Room (8:50 pm, Thursday)
Let me tell you, I didn’t realize how quickly they would get equipment ready and break the bag of waters!
We made the call to break the bag. I stepped into the restroom to pee, and by the time I got back out they were right in the middle of the procedure there on the bed!
Thankfully, after this, they moved us to an actual labor and delivery room down the hall. We hoped that things would start to pick up, which was the goal of breaking the bag of waters, after all…
Slow Down (9:00 pm, Thursday – 12:00 am, Friday)
However, things slowed back down. This did allow Rachel to take a shower and sleep for another hour or so, but it was concerning that we appeared to be moving backward.
As Rachel slept for a while, Teri sat in the recliner in the corner and I laid down on the couch.
I couldn’t sleep at all. I was watching her contractions get slower and slower on the monitor and wondering how much longer this process was going to go on for. I mean, sure, Rachel is a BOSS. But everyone has their limits. How much longer of an induction/labor process would she be able to take?
After she got some rest, we got Rachel up and moving around. Her and I took a couple laps around the Labor and Delivery unit.
Pick Back Up (12:00 – 2:30 am, Friday)
Thankfully, the movement and changing positions got things going again.
Honestly, I don’t remember too much about this period. I was purposefully just trying to stay awake and not pay too much attention to the clock.
At one point, however, after trying out various positions, we got Rachel into a good groove of contractions while she sat upright, cross-legged, in the bed—like some sort of pregnant zen master!
At 2:30am, they checked Rachel again. She was dilated to (*tired drumroll*) … 5cm.
My heart kind of sank at this point, because I didn’t know whether to expect things to really get moving, or to expect that we would spend all day/night Friday in labor.
Three Hours in Hell (2:30 – 5:30 am, Friday)
Thankfully, things really started to move along.
Granted, I say “thankfully,” but this was really the most intense three hours of the whole process.
The midwife who was on at that point was willing to allow Rachel to labor for awhile in the tub, which she was looking forward to.
However, because Rachel was on Pitocin, she was on continuous fetal monitoring… these two sensors they put around her stomach, to measure contractions and the baby’s heart rate.
Now, I don’t doubt that these monitors can prove incredibly helpful. But they can also be really freaking annoying. It is so easy to lose the baby’s heart rate whenever the mom moves. Then a nurse has to come back in and readjust the monitor until they find the heart rate again. But then mom or baby moves like two minutes later and the cycle begins again.
So, before they were going to let Rachel get in the tub, they wanted her to lie down on her back in the bed so that they could get a good 30 minutes of the baby’s heart rate on the monitor to make sure things were OK.
Rachel was not happy about this because lying on her back was the least comfortable position for her to be in. However, she endured, and made it to the tub.
The tub is where, eventually, Rachel got to “transition” or “transitional labor.” You can read more about it here. Suffice it to say that it’s usually the most intense part of labor.
Things were a blur by this point: Tub. Toilet. Tub. Bed. Birthing Ball. Tub. Vomit/retching.
At one point, between the hunger, exhaustion, the deep breathing I was doing with Rachel during her contractions, and kneeling beside the tub holding the puke bucket as she vomited…I began to get nauseous myself!
I asked Teri to go grab me a ginger ale, and I snuck swigs of ginger all and bites of a Clif Bar between Rachel’s contractions in the tub.
Again, at this point, I was purposefully trying not to pay attention to the clock. Sure, things seemed to be moving along now. I’d read in the books that when the mom said “I can’t do this anymore,” that usually meant they were in transition, which meant they were about ready to push…
But, at 2:30 am Rachel had only been at 5 centimeters. So, it didn’t seem wise to get my hopes up. And yet, here my wife was, throwing up over the side of the tub during contractions and saying she didn’t know how much longer she could do this for.
Somewhere around 5:15–5:30, the midwife and her student came in and checked Rachel again, because she was complaining of increased pressure down low.
At this point, I was praying that she was at least 8cm dilated. If not, based on how intense things had just gotten, I wasn’t sure how much longer Rachel would make it without, at the very least, some nitrous gas for pain management.
However, thanks be to God, she was dilated to…9.5cm!
“BUT I HAVE TO PUSH!” (5:30–5:46 am, Friday)
Now, if you’re in the know, you realize that 9.5cm doesn’t quite cut it. 10cm is the magic dilation number.
SO, although I personally took the 9.5cm news as a comforting blessing and relief from the Lord, for Rachel things got more intense for a bit.
As it’s been described to me, every fiber of her being was urging her to push that baby out, but I and everyone else in the room were urging her NOT to push until she reached full (10cm) dilation.
I was feeling: “YES! Thank God! We’re almost there! We don’t have to endure another full day of labor!!”
They turned the lights up in the room as more people entered to get things ready for delivery. Teri and I focused on keeping Rachel from pushing for as long as we could.
Eventually, the midwife went to check Rachel’s dilation again, and said: “Aaaand, the baby’s head is already through the cervix!”
Rachel: “DOES THAT MEAN I CAN PUSH?!”
Midwife: “Yep! You can push!”
Rachel only ended up pushing for 10-15 minutes.
Now, I usually don’t do well with blood, etc., but for some reason I was perfectly fine watching the whole thing as our daughter came out. It was wild. It took awhile to see her head coming, but then, boom!, she was all the way out and screaming!
BABY ARRIVES: Eva Joy Steele was born at 5:46 am on Friday, July 20, 2018.
She weighed 5lbs 8oz, she was 18 inches long, and she has been worth every minute of that lengthy labor and delivery!
Looking back, apart from the initial frustration about getting induced at 37 weeks, we felt very well cared for by the midwives and nurses at Elmhurst. We didn’t feel pressured into moving things along quicker than we felt comfortable with, and we’re very thankful for the medical care that Rachel and Eva received.
Also, we’re incredibly grateful to our doula, Teri, for her support along the way. Even if the only thing she had done was to turn the baby around, that would have been enough! But she went above and beyond throughout the rest of the process, and we’re very thankful she was there with us.
For me, after going through this with my wife, I’m even more impressed by what a strong woman she is. I already knew that she had grit, but making through such a long process without any kind of pain medication was nothing short of amazing.

With Rachel and Eva, I think we’ve got a pretty great team.
